Cancer remains one of the most significant global health concerns, affecting millions of lives each year. In 2020 alone, there were an estimated 19.3 million new cancer cases worldwide, and this number is projected to rise to 28.4 million by 2040. Sadly, cancer was responsible for approximately 10 million deaths globally in 2020, making it the second leading cause of death worldwide, accounting for nearly one in six deaths.
These numbers reflect not just the prevalence of cancer but also the immense physical, emotional, and financial toll it takes on patients and their families. The treatments used to combat cancer, such as chemotherapy and radiation, are powerful but can also be harsh on the body, leading to a range of side effects that can significantly impact a patient’s quality of life.
While modern medicine has made remarkable strides in improving survival rates for many types of cancer, the journey through treatment can still be grueling. This is where complementary therapies, like Hyperbaric Oxygen Therapy (HBOT), come into play. HBOT is not a cure for cancer, but it has been explored for its potential to support the body during cancer treatment, helping to manage side effects and promote overall well-being.
In this blog, we’ll explore how HBOT can be used as a supportive therapy during cancer care. We’ll explore its role in helping patients feel their best, aiding recovery, and potentially improving their quality of life as they navigate the challenges of cancer treatment.
What is Hyperbaric Oxygen Therapy (HBOT)?
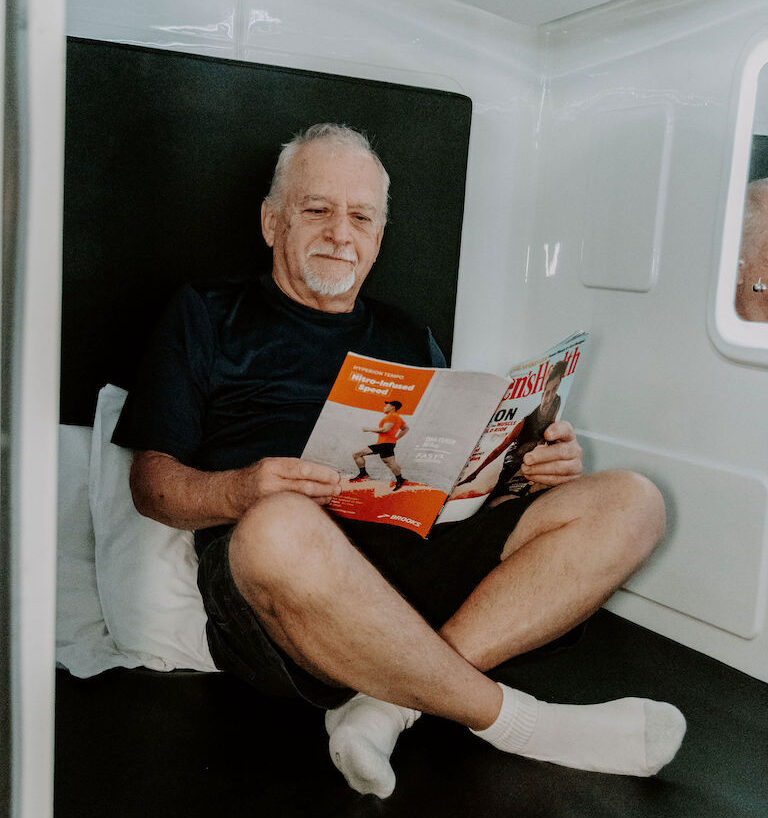
Hyperbaric Oxygen Therapy, commonly referred to as HBOT, is a medical treatment that involves breathing pure oxygen in a pressurized chamber. This treatment takes place in a specialized environment where the air pressure is significantly higher than normal atmospheric pressure. As a result, the lungs can absorb much more oxygen than they would under standard conditions.
This increased oxygen uptake allows the oxygen-rich blood to deliver higher levels of oxygen to tissues throughout the body. This can be especially beneficial in areas where the oxygen supply is typically limited, such as damaged or inflamed tissues. By flooding these areas with oxygen, HBOT can help accelerate the body’s natural healing processes, reduce inflammation, and promote tissue repair.
Originally, HBOT was developed to treat conditions like decompression sickness, which affects divers, and serious infections that are resistant to other treatments. Over time, however, its applications have broadened, and HBOT is now being explored for its potential benefits in various medical conditions, including as a supportive therapy during cancer treatment.
For cancer patients, whose bodies are often under significant stress due to the aggressive nature of treatments like chemotherapy and radiation, HBOT offers a way to help manage side effects and support overall health. While it’s not a cure for cancer, HBOT can play a complementary role in helping the body recover and maintain strength during this challenging time.
If you want more information on how HBOT works on a cellular level, check out our blog “Hyperbaric Oxygen Therapy: Understanding its Powerful Cellular Impact” here.
Enhancing Cancer Care with HBOT: Support Beyond Conventional Treatments
While traditional cancer treatments such as chemotherapy and radiation are critical in battling the disease, they often bring about side effects that can significantly diminish a patient’s quality of life. Hyperbaric Oxygen Therapy (HBOT) offers a complementary approach to mitigating these side effects. By enhancing oxygen delivery to tissue damaged by aggressive treatments, HBOT supports the body’s natural healing processes and promotes recovery, providing essential support to improve the overall well-being of cancer patients.
Managing Radiation-Induced Side Effects
Radiation therapy is a powerful tool against cancer but can harm healthy tissues near the treatment area. Hyperbaric Oxygen Therapy (HBOT) offers support in healing these tissues and managing side effects:
- Radiation Proctitis: Common in patients receiving radiation for pelvic cancers such as cervical, prostate, and bladder cancers, this painful inflammation of the rectum can significantly affect quality of life. HBOT helps reduce this inflammation and encourages tissue repair, easing discomfort and promoting recovery.
- Osteoradionecrosis of the Mandible (ORNM): This serious condition involves the deterioration of the jawbone following radiation for head and neck cancers, including oral and throat cancers. Incorporating HBOT as part of the treatment strategy can enhance tissue regeneration and lessen the severity of symptoms.
- Radiation-Induced Dysphagia: Often experienced by patients treated for head and neck cancers, difficulties in swallowing can severely impact nutrition and quality of life. HBOT may improve tissue healing and restore function, helping to alleviate these challenges.
Supporting Recovery from Surgery and Treatment
In addition to managing side effects, HBOT can play a significant role in supporting recovery from surgeries and treatments:
- Accelerating Wound Healing: Wound healing can be a major concern for cancer patients undergoing surgical procedures, especially in regions previously subjected to radiation therapy. HBOT enhances this healing process by significantly increasing the oxygen saturation in the tissues, which not only speeds up recovery but also minimizes the risk of post-surgical infections.
- Nurturing Surgical Flaps and Grafts: Reconstructive surgeries often involve the use of tissue flaps or grafts to repair areas affected by cancer removal. HBOT plays a crucial role by boosting oxygen levels in these critical tissues, ensuring their successful integration and survival. This support is vital for the overall success of reconstructive efforts, helping patients regain normalcy and function.
By optimizing tissue oxygenation, HBOT not only aids in swift recovery but also ensures that surgical interventions achieve the best possible outcomes, making it a valuable component of comprehensive cancer care.
Enhancing Quality of Life During Cancer Treatment
Hyperbaric Oxygen Therapy (HBOT) extends its benefits beyond treating specific side effects—it fundamentally enhances the overall well-being of cancer patients. By significantly improving oxygen transport across the body, HBOT helps mitigate some of the pervasive fatigue and general discomfort that often accompany cancer treatments. As a result, patients frequently report a noticeable boost in energy levels and an overall improvement in their quality of life. This uplift in well-being is crucial, empowering patients to handle their treatments with greater resilience and positivity..
Considerations for Integrating HBOT in Cancer Treatment
Hyperbaric Oxygen Therapy (HBOT) can be a valuable addition to a cancer treatment plan, offering support in managing the side effects of conventional therapies and promoting overall recovery. However, as with any complementary therapy, it’s important to approach HBOT with a clear understanding of its role and how it fits into an individual’s comprehensive cancer care strategy.
Individualized Care and Integration with Treatment
The benefits of HBOT can vary depending on the type of cancer, the specific side effects being addressed, and the overall treatment plan. HBOT is most effective when integrated into a personalized care approach tailored to the unique needs of the patient. Your healthcare team will work with you to determine how HBOT can best complement your existing treatments, ensuring that it supports your overall well-being and recovery.
Supporting Research and Ongoing Studies
HBOT has shown promise in helping to manage certain cancer-related side effects, particularly those associated with radiation therapy. While some applications are well-supported by current research, others are still being explored. Ongoing studies continue to expand our understanding of how HBOT can be used most effectively in cancer care, and your healthcare provider can help you stay informed about the latest developments. Unfortunately since research is still underway, HBOT is often not covered by insurance companies and patients typically have to pay out of pocket for services.
Enhancing Quality of Life During Treatment
The primary goal of incorporating HBOT into cancer care is to enhance your quality of life during and after treatment. By helping to reduce inflammation, promote healing, and support overall health, HBOT can play a significant role in making the treatment journey more manageable and less taxing on the body. It’s important to remember that HBOT is a supportive therapy—its value lies in how it complements your existing treatment plan, helping you feel your best as you navigate your cancer journey.
A Holistic Approach to Cancer Recovery
Navigating through cancer treatment is undeniably challenging, yet adopting a holistic approach, including therapies like HBOT, can significantly alleviate this journey. Although HBOT is not a standalone cure for cancer, its ability to enhance the body’s healing responses and support recovery makes it an invaluable part of a comprehensive cancer treatment strategy.
If you’re considering HBOT or seeking more information on how it can be integrated into your cancer care plan, our team at Michigan Health & Wellness is ready to assist. We are committed to devising a care strategy that not only addresses your immediate treatment needs but also supports your overall health and recovery, ensuring you have the best possible support throughout your cancer journey.
Contact us today to discuss how HBOT can enhance your treatment experience and help you achieve a better quality of life during and after cancer therapy.
Resources:
Costa, D. A., Amaro, C. E., Nunes, A., Cardoso, J. S., Daniel, P. M., Rosa, I., & Branco, J. V. (2021). Hyperbaric oxygen therapy as a complementary treatment for radiation proctitis: Useless or useful? – A literature review. World Journal of Gastroenterology, 27(27), 4413–4428. https://doi.org/10.3748/wjg.v27.i27.4413
Costa, D. A., Ribeiro, J. A., & Amaro, C. D. (2024). Hyperbaric oxygen therapy as a complementary treatment for osteoradionecrosis of the mandible: Useless or useful? – A literature review. https://www.semanticscholar.org/paper/Hyperbaric-Oxygen-Therapy-as-a-Complementary-for-of-Costa-Ribeiro/18a598a72902abfee68c50b85260e15931c5ce22
Lin, Z. C., Bennett, M. H., Hawkins, G. C., Azzopardi, C. P., Feldmeier, J., Smee, R., & Milross, C. (2023). Hyperbaric oxygen therapy for late radiation tissue injury. Cochrane Library, 2023(8). https://doi.org/10.1002/14651858.cd005005.pub5
The International Agency for Research on Cancer (IARC). (n.d.). Global Cancer Observatory. https://gco.iarc.fr/en